Were you diagnosed with a blighted ovum after undergoing an embryo transfer?
In this article you will learn:
- What is a blighted ovum,
- What causes it, and
- If it can prevented using IVF
What is a blighted ovum?
A blighted ovum (also known as an anembryonic pregnancy) is a pregnancy in which a fertilized egg successfully implants in your uterus, but the embryo does not develop.
It could also mean that an embryo was present on an initial ultrasound, but it gets resorbed, and only a gestational sac remains.
In this type of pregnancy, the placenta does develop and begins to produce the pregnancy hormone human chorionic gonadotropin (hCG).
This is why home pregnancy tests are still positive.
What are the causes of a blighted ovum?
We do not know the exact cause of a blighted ovum. We often think that there is some inherent genetic abnormality within the fertilized egg that does not allow it to develop appropriately.
We also cant determine if it’s coming from the maternal side (poor egg quality), the paternal side (poor sperm quality), or both.
Can a blighted ovum occur with in vitro fertilization?
Unfortunately, a blighted ovum can occur in any pregnancy, whether or not you’ve undergone fertility treatments.
Is blighted ovum more common with IVF?
A blighted ovum is not more common in IVF pregnancies. However, they are more likely to be detected in patients undergoing fertility treatment because of the increased use of early ultrasounds.
What is the percentage of having a blighted ovum after IVF?
An anembryonic pregnancy is a type of early pregnancy loss. It is estimated that early losses occur in about 10-15% of all pregnancies, IVF or not. However, this number may be underreported as many early miscarriages can go unnoticed.
Unfortunately, the incidence of developing any type of miscarriage increases with age.
How is it diagnosed?
An anembryonic pregnancy is diagnosed when an early pregnancy scan shows an empty gestational sac with no developing embryo.
Technically, there are strict diagnostic ultrasound findings which include:
- a gestational sac that measures greater than 25 mm with no embryo is diagnostic.
- there is no embryo ~10 days after a scan showed a gestational sac and a yolk sac
- there is no embryo ~14 days after a scan showed a gestational sac
Your blood tests will also be positive for the pregnancy hormone hCG.
What are my options? How is it treated?
There are three treatment options for any early pregnancy failure.
- Expectant management: Waiting for your body to pass the tissue naturally (aka a natural miscarriage).
- Medical management: A medication can be given to you to help you pass the tissue at home.
- Surgical management: A D&C procedure is done to remove all of the products of conception from your uterus.
Let’s go over the pros and cons of each management strategy.
Expectant Management
- Pros: The least invasive option: No intervention is needed
- Cons: There is a chance that your body won’t expel the tissue, and you’ll need to proceed with medical management or have a D&C procedure. The longer the nonviable pregnancy remains inside, the higher your risk of developing an infection.
Medical Management
- Pros: Medical management is less invasive than surgery and usually very effective in removing all of the products of conception. You can pass the pregnancy tissue in the privacy of your own home.
- Cons: It can be painful and last several hours. It also requires more follow-up, as you will need to return for a transvaginal ultrasound and blood work to ensure that the tissue has passed. Lastly, there is a chance that you won’t pass all of the tissue and will need to have a D&C procedure.
Surgical Management
- Pros: The most effective method in clearing the pregnancy. It is also the most efficient.
- Cons: It is a surgical procedure. Therefore, it requires an appointment, anesthesia and has a small risk of surgical complications.
Can I prevent it from happening again?
Unfortunately, there is no way to prevent a blighted ovum, but undergoing IVF with preimplantation genetic testing (PGT) may decrease the chances of having one.
However, the most basic form of genetic testing, PGT-A, will only look for a numerical chromosomal abnormality. (i.e., does the embryo have 46 chromosomes or not). It cannot detect other abnormalities like inversions or translocations.
Other related questions
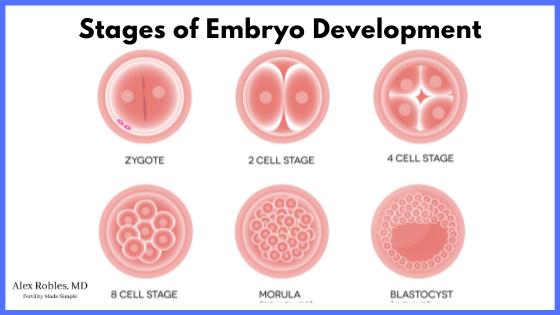
Can a blastocyst become a blighted ovum?
A blastocyst (an embryo that has grown to the 5th, 6th, or 7th days of development) can become a blighted ovum if it stops developing after implantation.
The same is true for a cleavage stage (Day 3) embryo.
Can a blighted ovum have a yolk sac?
A blighted ovum may or may not have a yolk sac.
To diagnose a blighted ovum, you only need:
- a sac greater than 25 mm in diameter with no embryo
- or the absence of an embryo 10-14 days after a previous ultrasound showed an empty sac.
Can a blighted ovum have a heartbeat?
Technically no. If a heartbeat was heard on an initial ultrasound and is no longer present at a follow-up ultrasound, this is considered a “missed abortion” or a missed miscarriage.
The treatment options are the same.
At what stage do blighted ova usually miscarry?
A blighted ovum can miscarry anywhere from 7-12 weeks of pregnancy. Most of the time, they pass naturally when an expectant management strategy is chosen, but this can take up to 8 weeks.
It may be a good idea to undergo some form of intervention to expedite the process.
Does a blighted ovum mean you are infertile?
A blighted ovum is a sign that there were problems with the early embryo. Although a prior loss puts you at a higher risk of having another loss, you are more likely to have a successful pregnancy with your next attempt than not.
However, if you have two or more miscarriages, this is considered recurrent pregnancy loss. Speak with your healthcare provider to learn if there is any work-up you need to have done.
Do you bleed with a blighted ovum?
Many women do not have any vaginal bleeding with a blighted ovum. Others may experience light spotting or brownish/pink spotting. If you begin to bleed heavier, you may be starting to pass the pregnancy tissue.
Other early pregnancy symptoms you might experience include:
- morning sickness
- sore breasts
- fatigue
What hCG levels do you typically see in a blighted ovum?
Typically, a blighted ovum will have an hCG level that is at the lower end of normal. However, the hormone levels will not rise appropriately as it does in a normal pregnancy.
Conclusion
A blighted ovum/anembryonic pregnancy is an early miscarriage likely due to chromosomal abnormalities in the embryo.
Unfortunately, we do not always know the underlying cause or how to prevent them from happening again.
However, it is essential to understand that nothing you have done caused it.
It is normal to experience grief, and we always encourage you to seek emotional support when needed.
Be sure to follow closely with your fertility specialist to determine your next step in achieving a healthy pregnancy.
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References:
- Chaudhry K, Tafti D, Siccardi MA. Anembryonic Pregnancy. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK499938/
- Nie QW, Hua R, Zhou Y, Li H, Yu YH. [Blighted ovum in subfertile patients undergoing assisted reproductive technology]. Nan Fang Yi Ke Da Xue Xue Bao. 2017 Jul 20;37(7):902-906. Chinese. DOI: 10.3969/j.issn.1673-4254.2017.07.08. PMID: 28736365; PMCID: PMC6765514.
- Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: a prospective register-based study. BMJ. 2019 Mar 20;364:l869. DOI: 10.1136/BMJ.l869. PMID: 30894356; PMCID: PMC6425455.
- Dugas C, Slane VH. Miscarriage. [Updated 2021 Jun 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532992/
