What does freeze all mean in IVF?
The term “freeze all” in IVF refers to the process of freezing or cryopreserving all the embryos you make in an IVF cycle, rather than transferring one or more of them into your uterus right away.
This only matters if you were planning to have a fresh embryo transfer, in which an embryo is placed into your uterus in the same cycle in which they were created.
Either way, any additional embryos that are not transferred are frozen anyway.
These embryos can remain frozen indefinitely and can be used at a later date in the future.
What are the advantages of freeze all cycles?
There are certain situations where a freeze-all cycle is advantageous or necessary.
Mitigates the risk of ovarian hyperstimulation syndrome
Ovarian hyperstimulation syndrome (OHSS) is a potentially serious complication that can develop during an IVF treatment cycle.
It occurs when your ovaries have a strong response to the ovarian stimulation (aka high responders). If you have polycystic ovarian syndrome, you are at increased risk of OHSS.
Symptoms are caused by fluid build-up inside the abdomen and other parts of the body, causing pain, bloating, nausea and vomiting.
While freezing the embryos does nothing to your risk of developing OHSS, it does protect you from experiencing a more severe form of the condition.
That’s because OHSS is worsened by b-HCG (human chorionic gonadotropin), the pregnancy hormone. If you happen to transfer one or more fresh embryos and get pregnant, your OHSS symptoms will significantly worsen.
In addition, you might also be able to prevent OHSS by freezing your embryos. Getting pregnant immediately following your egg retrieval could be the catalyst to spark the development in your body.
It decreases Endometrial dyssynchrony
The second way that freeze-all is advantageous is if your hormones aren’t in an optimal state to receive an embryo.
What does this actually mean?
The only time in which your body should produce high levels of progesterone is after you ovulate.
After ovulation, your progesterone level should rise as it is being produced by the corpus luteum (the cyst that contained the egg that you ovulated).
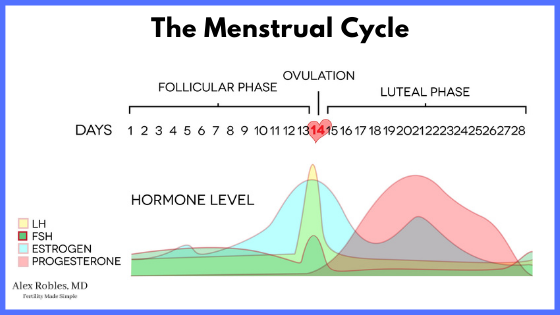
During this time, the egg and the sperm meet at the Fallopian tube and make their way down into the uterus over a span of 5 days.
This means that your uterus is exposed to progesterone for 5 days before an embryo has traveled from your Fallopian tube and into your uterine lining (aka the endometrium).
If your progesterone levels happen to become elevated before you ovulate, this will throw off the timing and synchrony between your endometrium and your hormone levels.
We use a cut-off of 1.5 ng/mL.
If your progesterone is higher than 1.5 ng/mL before your egg retrieval (aka ovulation day), then there may be a shift in your endometrial receptivity, and we do not recommend that you undergo a fresh embryo transfer.
It optimizes The endometrium
In addition, there is a chance that the lining of the uterus does not grow appropriately during an IVF cycle.
In general, we like to see a 7mm thickness to your endometrium with a triple stripe (trilaminar) appearance.
In addition, there shouldn’t be any fluid or blood in your lining which can have a negative impact on implantation rates.
If neither of these things is present by the time you have an egg retrieval, you should not undergo a fresh embryo transfer.
It Allows Pregnancy Planning for Medical reasons
You may also have a medical reason for freezing all of your embryos.
For example, cancer patients are often referred to a fertility specialist for emergency in vitro fertilization
The goal is to preserve fertility before undergoing cancer treatments which can potentially damage a woman’s uterus and reproductive potential.
There are other medical reasons too.
You might have a contraindication to getting pregnant right away, or perhaps you want to delay pregnancy to take care of a medical condition first.
In these situations, you can freeze all of your embryos and use them at some point in the future.
Or personal reasons
In addition, you may choose to freeze your viable embryos if you do not want to get pregnant right away. Perhaps you have other professional duties or extended travel coming up.
Embryo cryopreservation is a great way of delaying pregnancy for a more convenient time.
It allows for PGT testing
The last reason a freeze-all strategy is beneficial is if you are planning on doing preimplantation genetic testing.
Embryos that make it to the blastocyst stage are biopsied and frozen while the results of the genetic screening are awaited.
In general, biopsy results can take 10-14 days to return. In the meantime, your embryos will be frozen and safe.
Can all embryos / blastocysts be frozen?
All embryos can be frozen at any stage. An embryo can be frozen as early as the 2PN stage (which is Day 1), at the cleavage stage (Day 3), or the blastocyst stage (Days 5,6, or 7.)
Most people will freeze embryos at the blastocyst stage for three reasons.
- Blastocysts have the better chance of surviving a thaw and leading to a successful pregnancy.
- Blastocysts have already proven themselves to be able to grow past a certain level of development.
- Blastocysts can tolerate preimplantation genetic testing (aka embryo biopsy) better than embryos in earlier stages of development.
When can you use a frozen embryo?
A frozen embryo can be used at any time.
To use them, you will need to undergo a frozen embryo transfer cycle of FET for short.
A FET allows for additional time to prepare for pregnancy and allows for a better uterine environment prior to embryo transfer.
There are two types of FETs.
- A Natural Cycle FET
- A Medicated or Programmed FET
Either way, the goal is to transfer the embryo after your uterine lining has grown and has been exposed to progesterone.
What are the disadvantages of freezing your embryos?
What are the disadvantages of freezing your embryos?
First and foremost, freezing your embryos automatically indicates that you have to undergo a frozen embryo transfer.
The three main downsides to this are
- Increased cost
- Increased time to pregnancy
- Thawing
Doing a frozen embryo transfer entails another cycle of morning monitoring ultrasounds and blood work.
In addition, the embryo has to be thawed. These additional visits, analyses, and procedures will increase the cost of your treatment. There are also annual storage fees that need to be paid to keep your embryos frozen.
Secondly, you will have to wait at least another month after your egg retrieval before you can have the transfer.
Here’s an example of a Freeze all IVF cycle timeline:
- An IVF cycle lasts anywhere from 8-12 days, with the retrieval happening 36 hours after the last day of injections.
- It will then take ~2 weeks to get your period after the retrieval.
- Assuming you are cleared to do a frozen embryo transfer cycle right away, you will then come back on Days 2 or 3 of this next cycle.
- This will start another round of monitoring.
- Regardless of whether or not you do a medicated or a natural cycle, the embryo transfer will likely happen 2-3 weeks after this point.
You can learn more about a Frozen Embryo Transfer Timeline here.
Last but not least, a frozen embryo transfer requires that your embryo be thawed after freezing.
Although rare, there is a small chance that your embryo does not survive the thawing process.
I go over these 3 disadvantages of frozen embryo transfer in more detail in this post.
Other Related Questions
Are frozen IVF cycles more successful?
Some data indicate that frozen embryo transfers are more successful than fresh embryo transfers, however, some show no significant differences.
It all depends on the candidates chosen to have a fresh transfer.
For almost all intents and purposes, live birth rates can be equivalent between the two if you are a good candidate for a fresh transfer.
What is the success rate for frozen embryo transfer?
A PGT tested frozen embryo has approximately a 70-80% pregnancy rate and a 50-60% chance of yielding a live birth.
An untested embryo can have equal pregnancy rates and live birth rates if the embryo was created when the mother was under 35 years of age.
With that said, there are other factors to consider such as embryo quality and endometrial status.
Do frozen embryos take longer to implant?
Frozen embryos do not take longer to implant. We believe that implantation happens within 24-48 hours after the embryo transfer, regardless of whether or not you had a fresh or a frozen transfer.
How is this different from egg freezing?
Egg freezing uses the same technology (liquid nitrogen) as embryos to freeze or vitrify the cells.
The big difference between freezing embryos and eggs is that embryos have to be created in the lab before freezing them.
This process takes at least 5 days (if you are freezing at the blastocyst stage). Eggs however are frozen on the day that they are retrieved.
When they are thawed, eggs then have to go through the process of being fertilized and grown into embryos.
Conclusion
So in summary: a frozen embryo transfer can be an excellent choice for you if you need to delay pregnancy for medical or personal reasons.
Success rates can be equal or even better with a frozen embryo transfer cycle compared to a fresh transfer.
If you have been told by your doctor that you should have a freeze-all cycle, you now know what the risks, benefits, and alternatives include.
In addition, if you are fortunate enough to have produced multiple embryos, any extra embryo that isn’t transferred has to be frozen regardless.
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References:
- El Tokhy O, Kopeika J, El-Toukhy T. An update on the prevention of ovarian hyperstimulation syndrome. Womens Health (Lond). 2016;12(5):496-503. doi:10.1177/1745505716664743
- Griffiths AN, Watermeyer SR, Klentzeris LD. Fluid within the endometrial cavity in an IVF cycle–a novel approach to its management. J Assist Reprod Genet. 2002 Jun;19(6):298-301. doi: 10.1023/a:1015785431828. PMID: 12166637; PMCID: PMC3455216.
- Han AR, Park CW, Lee HS, Yang KM, Song IO, Koong MK. Blastocyst transfer in frozen-thawed cycles. Clin Exp Reprod Med. 2012;39(3):114-117. doi:10.5653/cerm.2012.39.3.114
- Roque M, Haahr T, Geber S, Esteves SC, Humaidan P. Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: a systematic review and meta-analysis of reproductive outcomes. Hum Reprod Update. 2019 Jan 1;25(1):2-14. doi: 10.1093/humupd/dmy033. PMID: 30388233.