In this article, you will learn the step-by-step process for an intrauterine insemination (IUI) procedure.
Specifically, you will learn:
- How long the process takes from start to finish
- What you should do to prepare for an IUI
- When to consider doing in vitro fertilization (IVF) instead
Let’s get started.
What is the step-by-step process of IUI?
The IUI process (also known as artificial insemination) involves the following seven steps:
- The initial consultation with a fertility specialist
- Undergoing the necessary workup to determine if you are a good candidate for IUI
- Scheduling a baseline ultrasound on Day 2-5 of your menstrual cycle to begin the IUI cycle
- Returning to the office periodically to monitor the growth of your follicle(s)
- Careful monitoring of your ovulation
- The actual IUI procedure
- Checking a pregnancy test ~2 weeks later
Let’s go over each step in detail.
1) Consulting with a fertility specialist
The first step is to schedule a consultation with a fertility specialist. The doctor will review your medical history, perform a physical exam, and discuss whether you are a potential candidate for IUI.
2) Undergoing the fertility workup
If you and your doctor determine that IUI may be a good option for you, the next step will be to undergo the necessary infertility workup.
The most common tests include:
Ovarian reserve testing
Ovarian reserve testing helps determine the number of eggs you have left in your ovaries. Testing often includes an AMH blood test and looking at your antral follicle count on an ultrasound.
Transvaginal Ultrasound
A transvaginal ultrasound gives us information about your anatomy, including the size and shape of your uterus, the appearance of the uterine lining, and the number of follicles in each ovary.
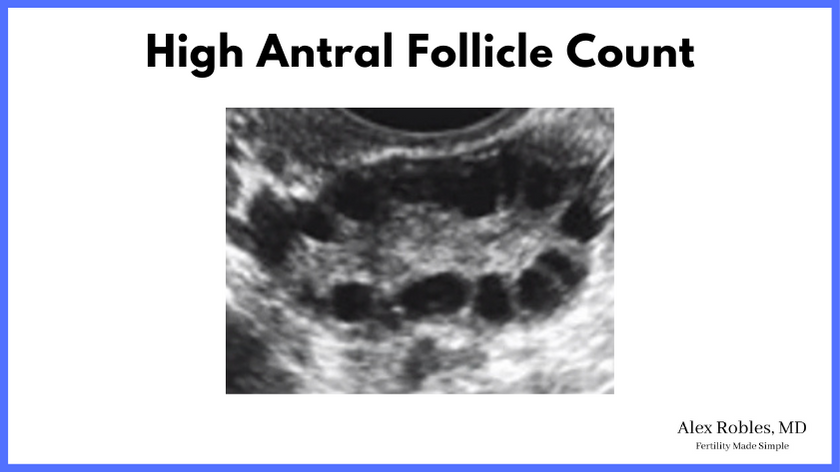
This ultrasound is usually done on Days 2-3 of your menstrual cycle to establish a baseline. We also check blood work to look at your Follicle Stimulating Hormone (FSH) and Estrogen Hormone level, which also provides information on your ovarian reserve.
Hysterosalpingogram (HSG)
An HSG is an x-ray of the uterus and pelvis that helps determine if your fallopian tubes are open or blocked. Open tubes are an absolute requirement for an IUI.
The HSG also looks at the uterine cavity to determine if any structural abnormalities might interfere with implantation inside the uterus.
Other Hormonal Blood Tests
In addition to AMH, your doctor will also order a Thyroid Stimulating Hormone test (TSH) and possibly a Prolactin level. An abnormality in either of these hormones might interfere with ovulation, a common cause of infertility.
Semen Analysis (if applicable)
A semen analysis is also done on the male partner to determine if there is an issue with sperm quality that could impact IUI success rates.
Specifically, a low sperm count will likely have the most significant impact.
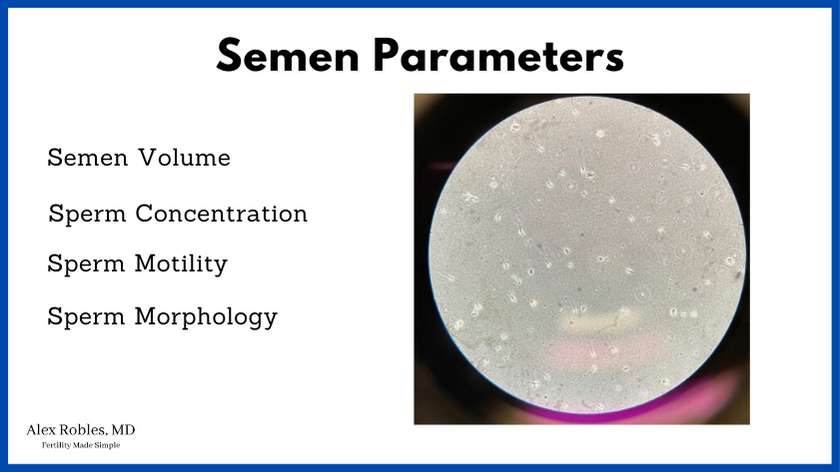
If you do not have a male partner, you will need to obtain donor sperm from a reputable sperm bank to proceed with an IUI.
3) Scheduling a baseline ultrasound on Days 2-5 of your menstrual cycle
Once you complete the fertility workup, your doctor will review your test results and discuss if IUI is a good option for you.
If so, you will be instructed to come in and schedule an ultrasound for Days 2, 3, 4, or 5 of your menstrual cycle. Most patients come in on day 3.
We will check your follicles sizes on each ovary, measure your uterine lining, and check your hormone levels at this visit. If everything comes back normal, you will begin the IUI cycle.
4) Monitoring the growth of the follicle(s)
At this point, you may or may not start oral medications to help your follicle grow. A standard medicated IUI cycle will begin with 50 mg of Clomiphene Citrate (aka Clomid) for five days.
If you have PCOS, you will start oral Letrozole for five days.
After taking the oral medications for five days, you will return to the office in ~3 days for another ultrasound to check the growth of your follicle(s).
If your follicles are growing but not yet ready for IUI, you will be asked to come back for another ultrasound in 1-3 days.
5) Careful monitoring of your ovulation
Once your follicle(s) have reached an appropriate size for ovulation (~20 mm), your doctor will have you take an hCG trigger shot that evening.
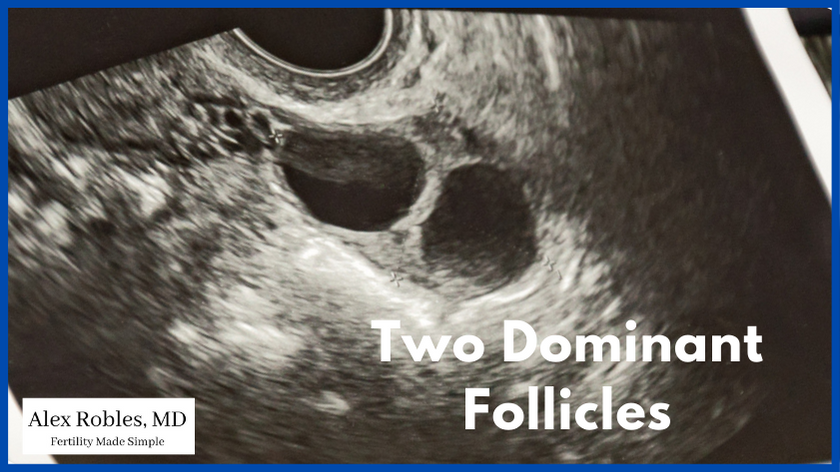
This injection mimics the natural LH surge that occurs in a regular menstrual cycle and leads to ovulation in ~36 hours.
If your body is already showing signs of getting ready to ovulate (i.e., your LH levels were rising), your doctor may choose not to give you the hCG trigger, and your IUI may be scheduled for the following day.
6) The actual IUI procedure
You will be instructed to come into the office on the morning of the planned IUI. (Usually, 36 hours after your hCG trigger shot, or 24 hours after a rise in LH hormone was detected).
If you have a male partner, he will be instructed to provide a fresh semen sample that is prepared for the procedure. If a frozen sperm sample is already stored at the office, the andrology team will begin preparing the sperm.
The actual IUI procedure is often very straightforward.
- You will sign a consent form detailing the risks and benefits of the IUI procedure
- You will then be asked to confirm your name and date of birth and confirm the sperm sample.
- A speculum is placed in your vagina to visualize your cervix, similar to a pap smear
- The thin and flexible IUI catheter is passed through your cervix and into the lower uterine segment.
- The sperm is then pushed through the thin tube of the catheter into your uterus.
- The catheter is withdrawn, and the procedure is over
You do not have to stay lying down in the office for observation, and you can go about your normal day right after. We also encourage you to have sexual intercourse the same day if possible to increase the number of sperm in the uterine cavity.
It is not uncommon to have light spotting and mild cramping after the procedure.
7) Checking a pregnancy test ~2 weeks later
After this point, there is nothing left for you to do. The hope is that one sperm finds its way into the fallopian tube and successfully fertilizes your ovulated egg.
You won’t know if the process was successful until you check a home pregnancy test ~2 weeks later.
If you do not get a positive result, or if you get your period, the cycle failed.
However, if you do have a positive test result, congratulations! You will then be asked to come into the office for a confirmatory beta HCG blood test.
How long is the IUI process from start to finish?
The actual IUI procedure takes only about ~10 minutes.
The entire IUI cycle, from the first office visit to the procedure, can range anywhere from 9-15 days.
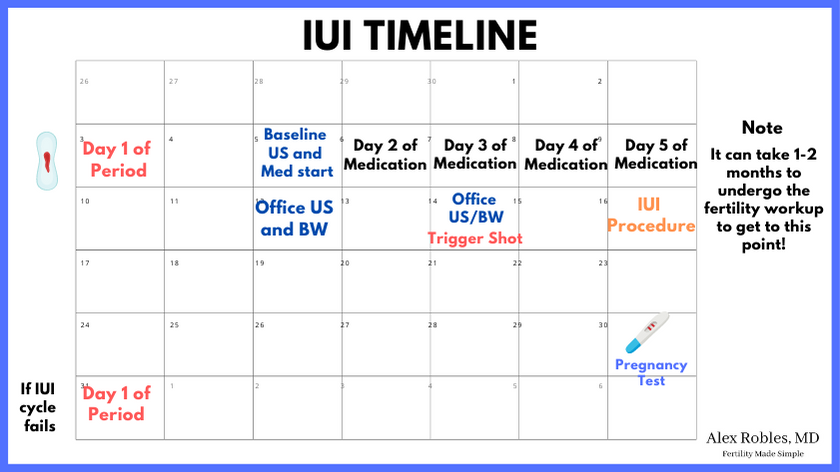
Here is an example calendar of what the IUI process looks like:
- Months 1-2: Consultation and fertility work-up
- Day 1: On Day 1 of your period, call to schedule your Day 3 visit
- Day 3: Your baseline ultrasound and bloodwork, and start of medications
- Days 4-7: Oral medications once a day
- Day 10: Monitoring visit for ultrasound and bloodwork
- Day 12: Monitoring visit for ultrasound and blood work, and trigger shot
- Day 14: The IUI Procedure
- Day 28: Pregnancy testing
How should you prepare for IUI treatment?
The best ways to prepare for an IUI include:
- Eat a healthy, well-balanced diet
- Avoid excessive alcohol
- Do not smoke
- Engage in some physical activity
- Maintaining a healthy BMI
- Doing your best to avoid excessive stress
How long after the IUI do you ovulate?
It is difficult to know the exact time that you will ovulate, but the goal is to perform the IUI at or around the time of ovulation. It is still possible to get pregnant from an IUI that occurs after you have already ovulated.
In general, many patients will ovulate ~36 hours after an hCG trigger shot.
How do you track ovulation with IUI?
Your reproductive endocrinologist will check an LH blood test at every office visit to look for any signs of impending ovulation. In addition, you can check ovulation predictor kits at home, which can also detect a rise in LH hormone in your urine.
How many IUI does it take to get pregnant?
In general, most successful IUI pregnancies will occur in the first 3-4 cycles. Studies demonstrate that approximately 90% of all IUI pregnancies occur by the fourth cycle.
The reported success rate for an IUI cycle ranges from 10-15% per cycle; however, the chances of success decrease with increasing maternal age.
After 3-6 failed IUI cycles, it is more time-efficient (though more cost-prohibitive) to proceed with in vitro fertilization.
Some insurance companies also require that you undergo a certain number of IUIs before covering other forms of infertility treatment.
How should you sleep after IUI?
There is no data to support that sleeping in any particular position after an IUI affects the outcome.
The best position to sleep after IUI is the one you are most comfortable with.
What is The Typical Cost of an IUI Procedure?
The typical cost of an IUI cycle (without medications) is about ~$500-$2000.
Insurance coverage varies, and some cycles require more visits or more extensive testing.
Conclusions
The entire step-by-step IUI process can take approximately 2 months, while the procedure itself takes only ~10 minutes.
IUI can be an effective procedure in helping couples achieve pregnancy, especially those struggling with ovulatory disorders or unexplained infertility.
In general, you should plan on doing ~3 cycles of IUI before deciding to move on to other fertility treatments.
Keep Reading:
- When Should You See A Reproductive Endocrinologist? [A Helpful Guide]
- IUI vs IVF: What is the Difference and Which Should You Do?
- What is Letrozole: Fertility Drugs Explained
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References:
- Dickey, R. P., Pyrzak, R., Lu, P. Y., Taylor, S. N., & Rye, P. H. (1999). Comparison of the sperm quality necessary for successful intrauterine insemination with World Health Organization threshold values for normal sperm. Fertility and sterility, 71(4), 684–689. https://doi.org/10.1016/s0015-0282(98)00519-6
- Allahbadia GN. Intrauterine Insemination: Fundamentals Revisited. J Obstet Gynaecol India. 2017;67(6):385-392. doi:10.1007/s13224-017-1060-x
- Morshedi M, Duran HE, Taylor S, Oehninger S. Efficacy and pregnancy outcome of two methods of semen preparation for intrauterine insemination: a prospective randomized study. Fertil Steril. 2003 Jun;79 Suppl 3:1625-32. doi: 10.1016/s0015-0282(03)00250-4. PMID: 12801569.
- Soria M, Pradillo G, García J, Ramón P, Castillo A, Jordana C, Paricio P. Pregnancy predictors after intrauterine insemination: analysis of 3012 cycles in 1201 couples. J Reprod Infertil. 2012 Jul;13(3):158-66. PMID: 23926541; PMCID: PMC3719352.
