PGS aka PGT (preimplantation genetic testing) is a method of screening embryos for genetic mutations before implanting them into your uterus.
In this post you’ll learn:
- What exactly PGT testing tells you,
- PGS testing statistics by age, and
- What to expect in terms of reliability and success rates.
Let’s get started.
*Note: PGS stands for preimplantation genetic screening. This term has been replaced with PGT-A, or preimplantation genetic testing for aneuploidy. I will be using the terms interchangeably.*
What does PGS testing tell you?
Preimplantation genetic testing is meant to tell you if your embryo has a specific genetic abnormality or not. That way, you can avoid transferring an abnormal embryo which can lead to miscarriage or an unhealthy baby.
There are three different types of preimplantation genetic tests, each looking at three different things: PGT-A, PGT-M, and PGT-SR.
PGT-A
PGT-A is the most common form of preimplantation testing and it looks for something called aneuploidy.
This is a fancy way of saying, does the embryo contain the correct number of chromosomes?
Humans have 23 pairs of chromosomes- equalling 46.
Therefore, an embryo with 46 chromosomes is called a ” euploid embryo ” and is considered normal.
Any other number than 46 is abnormal.
If the embryo is missing a chromosome and has 45, this is known as monosomy.
If it contains an extra chromosome and has 47, this is known as a trisomy.
An embryo could even have a monosomy on one chromosome and a trisomy on another one. It can also be a complex aneuploid, having multiple missing or additional chromosomes.
Mosaicism
PGT-A can also detect mosaicism.
Embryo mosaicism is when an embryo contains two or more genetically distinct cell lines.
For example, some cells appear chromosomally normal, while others showed some form of aneuploidy.
If you get a mosaic embryo, your clinic may or may not recommend transferring this embryo depending on your situation.
Oftentimes, we will recommend that you see a genetic counselor to understand the risks involved with using a mosaic.
So the potential results are:
- Euploid
- Aneuploid
- Mosaic
- No result (an insufficient amount of DNA was seen in the sample, so a result could not be determined).
PGT-M
PGT-M (preimplantation genetic testing for monogenic diseases) takes it one step deeper and screens for specific genetic conditions that affect individual genes. A gene is a segment of DNA that is located within a specific chromosome.
You would only do PGT-M if there is a genetic condition that runs in your family, or if you and your partner carry the same genetic disorder that you risk passing on to your offspring.
PGT-M cannot “fix” an embryo that has the condition. All we can tell you is that this particular embryo has or doesn’t have the condition.
PGT-SR
Preimplantation genetic testing for structural rearrangements looks for larger genetic defects.
Sometimes you may have something called a translocation or inversion mutation where parts of two different chromosomes are exchanged or even missing.
PGT-SR is less commonly used and is usually only done when a specific structural mutation is detected in either parent.
What abnormalities does PGS test for?
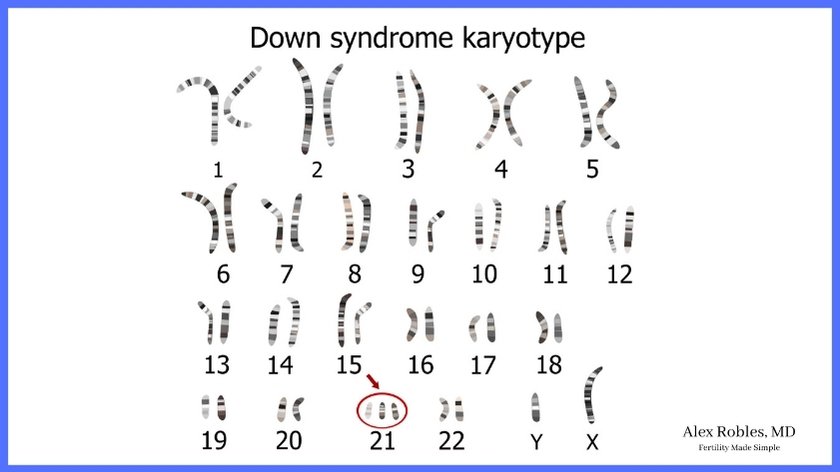
PGT-A only looks for numerical chromosomal abnormalities. This is useful for detecting common disorders like Down syndrome (which is trisomy 21) and trisomies 13 and 18.
It does not look for genetic conditions caused by single mutations in a gene.
PGT-M on the other hand tests for a specific genetic condition that may run in your family.
Common conditions it can screen for include cystic fibrosis, spinal muscular atrophy, Tay-Sachs disease, thalassemia, sickle cell anemia, Huntington’s disease, BRCA, and much more.
We have to know the specific condition that we are looking for to be able to do PGT-M.
Lastly, PGT-SR can test for larger genetic abnormalities like Robertsonian translocations or chromosomal inversions.
What percentage of PGS embryos are normal? (PGS Testing Statistics by Age)
In women under the age of 35, approximately 60% of embryos will be chromosomally normal.
In women between the ages of 35-38, only about 50% of embryos will be euploid.
The rate of aneuploidy begins to increase significantly after the age of 40 and drops below 30% in women over the age of 41.
This explains why miscarriage rates are significantly higher in women over the age of 40.
Increasing maternal age is associated with decreasing egg quality.
Is PGS testing reliable?
PGT-A is very reliable for detecting aneuploidy. It is reported to have ~ 95% accuracy.
With that said, nothing is ever 100%. PGT does not guarantee that you have healthy embryos.
In addition, there is a small chance that the embryo biopsy can lead to a
- False positive: The embryo is labeled as abnormal, but it is actually normal
- False negative: The embryo is labeled as normal, but it is actually abnormal
- Mosaic result: Mosaic embryos have been transferred and have led to seemingly normal babies. However, mosaic embryos do have as high of live birth rates compared to euploid embryos.
That is why we always recommend that you get some form of non-invasive prenatal aneuploidy assessment in early pregnancy at the very least.
Should I get PGS Testing?
Several studies have concluded that PGT-A can improve your chances of a live birth if you are 35 years of age or older.
In this patient population, PGT-A offers the benefit of choosing the single best embryo for the transfer. This decreases the time to pregnancy and increases the likelihood of achieving a live birth as abnormal embryos are more likely to lead to miscarriage.
However, PGT-A does not seem to improve overall pregnancy rates in women under the age of 35.
Other patients who benefit from PGS include:
- Couples with recurrent pregnancy loss (aka RPL or recurrent miscarriages)
- Couples with a known monogenic disorder
- Couples with a known structural chromosomal anomaly
It is important to note that PGT is optional, and will add costs to your IVF treatment cycle.
How long do PGS results take? (The Genetic Testing Timeline)
PGS results take between 10-14 days after the embryo biopsy is taken.
An average IVF cycle lasts between 8-12 days.
You will take a trigger shot on the last day of the cycle and your egg retrieval occurs 36 hours after the trigger.
Your eggs will be fertilized with sperm on that day.
The day following your retrieval, we will check to see if fertilization successfully took place. This is Day 1.
Your embryos will then be kept in the IVF lab for one week.
Hopefully, one or more embryos will make it to the blastocyst stage on Days 5, 6, or 7. This is when the biopsy will be performed and sent for genetic testing.

The embryo will then be frozen and can be used for a frozen embryo transfer in the future.
From this point, it will be 10-14 days until we receive the report of your genetic testing results.
Other Related Questions
Can PGS detect Down syndrome?
PGT-A can detect Down syndrome if it is present in the embryo. Instead of seeing two copies of chromosome 21, an embryo with Down syndrome will have three copies (Trisomy 21).
Can PGS detect autism?
PGT cannot detect autism because it is not caused by a single gene mutation or a chromosomal numerical abnormality.
As of right now, the exact cause of autism is unknown and thought to be due to multiple factors.
If autism is present in your family it is important to get a genetic carrier screening test to look for other conditions you might carry in your DNA.
Does PGS Testing Reveal Gender?
PGT-A can reveal the gender of an embryo by looking at the two sex chromosomes. If an embryo has two X chromosomes, it is a female. If an embryo has an X and a Y chromosome, it is a male.
Is PGS Safe?
The PGT biopsy is a fairly safe procedure when done on blastocyst embryos.
A blastocyst has two distinct cell lines :
- The outer cells, known as the trophectoderm, which is what will eventually form the placenta.
- The inner cell mass is what will form the embryo.
A PGT biopsy takes a small sample of 5-7 cells from the trophectoderm. However, a larger biopsy is taken, it can potentially harm the embryo.
While the risk of harm to the embryo is small, recent studies have seen a small increase in placental-related pregnancy complications in embryos that have undergone PGT biopsy.
This includes preeclampsia and other hypertensive disorders, and possibly small for gestational age fetuses.
Conclusion
No single test can accurately predict the risk of all possible defects in an embryo.
PGT is an optional test that can benefit women >35 years of age undergoing in vitro fertilization by avoiding the use of an aneuploid embryo.
Having a euploid embryo does not guarantee a live birth.
Be sure to speak with your doctor to learn about your individual risks and benefits and if PGT can help you achieve a healthy baby!
Related Articles
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References
- Demko ZP, Simon AL, McCoy RC, Petrov DA, Rabinowitz M. Effects of maternal age on euploidy rates in a large cohort of embryos analyzed with 24-chromosome single-nucleotide polymorphism-based preimplantation genetic screening. Fertil Steril. 2016 May;105(5):1307-1313. doi: 10.1016/j.fertnstert.2016.01.025. Epub 2016 Feb 8. PMID: 26868992.
- C. Hanson, T. Hardarson, K. Lundin, C. Bergh, T. Hillensjö, J. Stevic, C. Westin, U. Selleskog, L. Rogberg, M. Wikland, Re-analysis of 166 embryos not transferred after PGS with advanced reproductive maternal age as indication, Human Reproduction, Volume 24, Issue 11, November 2009, Pages 2960–2964, https://doi.org/10.1093/humrep/dep264
- Zhang L, Wei D, Zhu Y, Gao Y, Yan J, Chen ZJ. Rates of live birth after mosaic embryo transfer compared with euploid embryo transfer. J Assist Reprod Genet. 2019 Jan;36(1):165-172. doi: 10.1007/s10815-018-1322-2. Epub 2018 Sep 24. PMID: 30246223; PMCID: PMC6338591.
- Munné S, Kaplan B, Frattarelli JL, Child T, Nakhuda G, Shamma FN, Silverberg K, Kalista T, Handyside AH, Katz-Jaffe M, Wells D, Gordon T, Stock-Myer S, Willman S; STAR Study Group. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019 Dec;112(6):1071-1079.e7. doi: 10.1016/j.fertnstert.2019.07.1346. Epub 2019 Sep 21. PMID: 31551155.
- Neal, S. A., et al. “High cellularity of trophectoderm biopsy adversely affects pregnancy outcomes.” Fertility and Sterility 102.3 (2014): e176-e177.
