What is the difference between IVF and ICSI?
In this post, you will learn
- When it is better to use ICSI,
- The pros and cons of ICSI,
- If ICSI affects embryo quality, congenital defects, or gender
Let’s get started.
What Is The Difference Between IVF and IVF with ICSI?
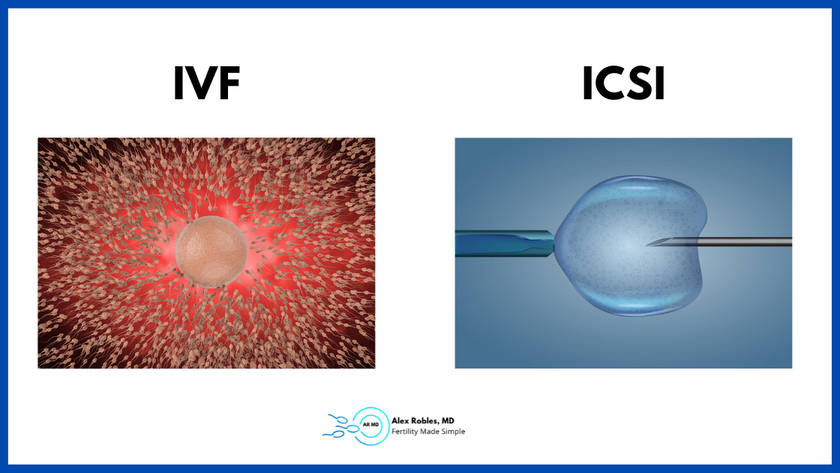
The main difference between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) is the method used to fertilize the egg.
With IVF (aka conventional insemination), numerous sperm are placed in a dish together with the eggs and allowed to fertilize naturally.
In ICSI, a single sperm is injected into each egg using a tiny needle.
IVF simulates what happens during natural fertilization. Hundreds of sperm are allowed to interact with the egg, but only one enters.
Which Is Better?
ICSI is the better option in cases of male factor infertility. It may improve fertilization rates when there are low numbers of sperm or poor sperm quality on semen analysis.
ICSI may also be the better option in cases where conventional insemination has led to failed or lower than expected fertilization rate in a previous IVF cycle.
Lastly, ICSI may also increase fertilization rates in couples with unexplained infertility. However, it is unclear if these patients have improved live birth rates.
With that said, ICSI does not guarantee that the egg will fertilize or that the embryo will be of good quality.
Is IVF More Successful With ICSI?
ICSI can improve the success rate of IVF, particularly in cases of male factor infertility or poor fertilization in a prior cycle.
Some fertility clinics routinely use ICSI in most patients as the likelihood of a complete failed fertilization is low with ICSI.
However, the routine use of ICSI in cases without male factor infertility or poor fertilization rates has not been shown to improve overall success rates (Study 1)(Study 2).
What Percentage Of Eggs Fertilize With ICSI? (Success Rates)
Approximately 50 to 70 percent of eggs will fertilize with ICSI. Lower fertilization rates may be seen in older women, those with fewer eggs, or when the sperm is of very poor quality.
What Are The Disadvantages Of ICSI?
ICSI may increase the risk of some complications, such as birth defects and genetic abnormalities on rare occasions.
One study of over 308,000 births, of which 6,100 came from IVF or IVF/ICSI, noted that couples who underwent ICSI had an increased risk of birth defects. The IVF group did not appear to have an increased risk.
However, it is unclear if the defects are due to the ICSI itself or to the underlying infertility issues in the men that necessitated ICSI in the first place.
The second disadvantage of ICSI is that the procedure may damage the egg. Oocyte degeneration can occur due to the ICSI technique or an inherent defect in oocyte quality.
Lastly, ICSI increases the cost of an already costly process.
What Birth Defects Do You See in ICSI VS IVF?
Several studies have found an association between IVF/ICSI children with a modestly increased risk of genitourinary, cardiovascular, musculoskeletal, and gastrointestinal abnormalities.
It is important to note that the absolute risk of birth defects is still low, and most children born through ICSI cycles are healthy. The risk of congenital malformation for children conceived through IVF/ICSI is about 7%, compared to 4% in the general population.
One of the most common abnormalities is hypospadias – when the opening of the penis (the urethra) is not at the tip of the penis and is typically on the underside of the penis.
Are ICSI Babies Healthy Otherwise?
Studies of children conceived through ICSI have found no significant difference in psychological, neurological, cognitive, and pubertal outcomes compared to children conceived spontaneously. (Study 1) (Study 2).
Can ICSI Babies Have Babies?
ICSI babies can have children of their own. In general, ICSI does not affect the fertility of the child. There are some exceptions, such as cases in which male offspring inherit a Y chromosome microdeletion from their father.
Do You Need to Do ICSI in Cases of Preimplantation Genetic Testing?
Preimplantation genetic testing (PGT) is a procedure used to screen for genetic abnormalities in the embryo before we transfer it back to the uterus.
PGT-A, also called aneuploidy screening, screens for the most common chromosomal abnormalities. PGT-M is used to test for specific genetic mutations that may be present in either parent.
Many fertility doctors argue that ICSI can make the PGT-A more accurate. In IVF, millions of sperm surround each egg. In theory, sperm that attached to the egg but didn’t fertilize the egg may leave some residue, which can alter the results.
On the other hand, ICSI is required for PGT-M as the specific genetic mutation being tested for may be present in one sperm, not another. As such, excess genetic material from other sperm cells can certainly invalidate the results.

Other Related Questions
Does ICSI Improve Embryo Quality?
ICSI does not improve embryo quality. ICSI helps improve fertilization rates in cases of poor sperm quality or quantity. It does not improve the quality of the embryo.
Does ICSI Increase The Chance Of Twins?
ICSI does lead to a slight increase in the risk of monochorionic twins for unknown reasons. The theory is that the artificial opening created by ICSI may cause the embryonic mass to split.
Does ICSI Cost More Than IVF?
ICSI is more expensive than IVF because it is a more complex procedure. It requires additional laboratory expertise, experience, resources, and time.
On the other hand, conventional insemination is a more straightforward procedure in which the sperm and the eggs are incubated in a petri dish overnight.
Does ICSI Affect Gender?
ICSI appears to lead to a slightly higher incidence of female infants than IVF. However, IVF treatment generally leads to a higher male-to-female ratio after a day five blastocyst transfer. The reason is that embryos are selected for transfer based on morphological appearance and how quickly they divide. Male embryos may develop quicker than female embryos and thus, are more likely to be chosen.
Does ICSI Cause Autism?
There is some evidence associating ICSI with autism; however, the increased risk appears to be due to the higher likelihood of adverse pregnancy and birth outcomes. Babies born through assisted reproductive technologies (ART) are more likely to
- be born prematurely,
- have a low birth weight,
- or be part of a multiple gestation (twins, triplets, etc.).
How Many Sperm Do You Need For ICSI?
ICSI doesn’t require as many sperm as IVF. With ICSI, only one motile sperm is needed for each egg.
That is one of the main reasons why ICSI benefits men with a low sperm count or poor sperm quality.
In addition, the embryologist picks the best sperm they can identify for ICSI use.
How Do Embryologists Pick Sperm For ICSI?
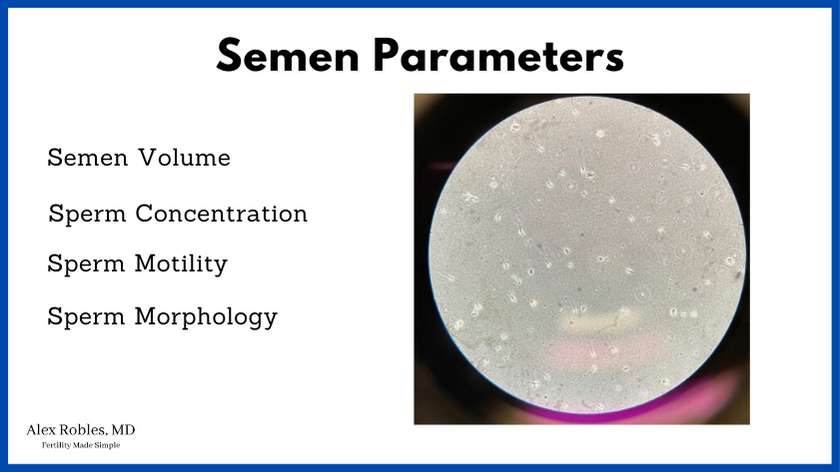
Embryologists place the semen sample under a microscope to assess the number of sperm present in the sample, their shape, and their motility.
Sperm that have normal morphology and good forward motility are chosen for the ICSI process.
Does ICSI Increase The Chance Of Down Syndrome?
ICSI does not increase the risk of Down syndrome. Chromosomal aneuploidies like Down syndrome are more likely due to advanced maternal age.
Does ICSI Work The First Time?
Unfortunately, ICSI treatment does not guarantee success the first time. Many variables affect success rates, such as the age of the female, the number of eggs retrieved after ovarian stimulation, the medical history, the quality of the eggs, and the infertility diagnosis in both parents.
Summary of The Pros And Cons Of ICSI
Pros of ICSI:
- ICSI can improve fertilization rates in men with poor sperm quality or quantity or in cases with failed fertilization in a previous cycle.
- ICSI can be beneficial in cases of preimplantation genetic testing (PGT) as it minimizes the risk of contamination from other sperm.
- ICSI is a relatively low-risk procedure with a high success rate
Cons of ICSI:
- ICSI may increase the risk of birth defects or genetic abnormalities. However, the absolute numbers are small, and the risk is likely not due to the ICSI procedure itself.
- ICSI incurs an additional cost to IVF.
- ICSI may increase the risk of monozygotic twins.
Final Words: Should You Do ICSI With IVF?
The decision to do an ICSI cycle should be made on a case-by-case with your fertility specialist.
If you have poor sperm quality or quantity, or if you’ve had failed fertilization in the past, ICSI may benefit you. However, current evidence does not support the routine use of ICSI in non-male factor cases.
Related Articles:
- IVF Vs IUI (Intrauterine Insemination): What Is The Difference Between The Two Most Common Fertility Treatments?
- How Long Does Traditional IVF Take? Step-by-Step Timeline
- The Embryo Transfer: What To Expect and What Not To Do
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References:
- Eftekhar M, Mohammadian F, Yousefnejad F, Molaei B, Aflatoonian A. Comparison of conventional IVF versus ICSI in non-male factor, normoresponder patients. Iran J Reprod Med. 2012 Mar;10(2):131-6. Erratum in: Int J Reprod Biomed. 2021 Apr 22;19(4):391. PMID: 25242986; PMCID: PMC4163275.
- Bhattacharya S, Hamilton MP, Shaaban M, Khalaf Y, Seddler M, Ghobara T, Braude P, Kennedy R, Rutherford A, Hartshorne G, Templeton A. Conventional in-vitro fertilisation versus intra-cytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet. 2001 Jun 30;357(9274):2075-9. DOI: 10.1016/s0140-6736(00)05179-5. PMID: 11445099.
- Ludwig M, Katalinic A, Gross S, Sutcliffe A, Varon R, Horsthemke B. Increased prevalence of imprinting defects in patients with Angelman syndrome born to subfertile couples. J Med Genet. 2005 Apr;42(4):289-91. DOI: 10.1136/jmg.2004.026930. PMID: 15805153; PMCID: PMC1736039.
- Davies MJ, Moore VM, Willson KJ, Van Essen P, Priest K, Scott H, Haan EA, Chan A. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012 May 10;366(19):1803-13. DOI: 10.1056/NEJMoa1008095. Epub 2012 May 5. PMID: 22559061.Källén B, Lauritsen J. IVF and ICSI increase the risk of birth defects in singletons and twins. Hum Reprod. 2012 Jul;27(7):2241-50. DOI: 10.1093/humrep/des135. Epub 2012 May 14. PMID: 225
- Alukal JP, Lamb DJ. Intracytoplasmic sperm injection (ICSI)–what are the risks? Urol Clin North Am. 2008 May;35(2):277-88, ix-x. DOI: 10.1016/j.ucl.2008.01.004. PMID: 18423248; PMCID: PMC2424218.
- Lacamara C, Ortega C, Villa S, Pommer R, Schwarze JE. Are children born from singleton pregnancies conceived by ICSI at increased risk for congenital malformations when compared to children conceived naturally? A systematic review and meta-analysis. JBRA Assist Reprod. 2017 Sep 1;21(3):251-259. DOI: 10.5935/1518-0557.20170047. PMID: 28837036; PMCID: PMC5574649.
- Skiadas CC, Missmer SA, Benson CB, Gee RE, Racowsky C. Risk factors associated with pregnancies containing a monochorionic pair following assisted reproductive technologies. Hum Reprod. 2008 Jun;23(6):1366-71. DOI: 10.1093/humrep/den045. Epub 2008 Mar 31. PMID: 18378561.
- Glenn TL, Kotlyar AM, Seifer DB. The Impact of Intracytoplasmic Sperm Injection in Non-Male Factor Infertility-A Critical Review. J Clin Med. 2021 Jun 14;10(12):2616. DOI: 10.3390/jcm10122616. PMID: 34198564; PMCID: PMC8231975.
- Fountain C, Zhang Y, Kissin DM, Schieve LA, Jamieson DJ, Rice C, Bearman P. Association between assisted reproductive technology conception and autism in California, 1997-2007. Am J Public Health. 2015 May;105(5):963-71. DOI: 10.2105/AJPH.2014.302383. Epub 2015 Mar 19. PMID: 25790396; PMCID: PMC4386543.
- Linens L, Celestin-Westreich S, Bonduelle M, Liebaers I, Ponjaert-Kristoffersen I. Follow-up of cognitive and motor development of 10-year-old singleton children born after ICSI compared with spontaneously conceived children. Hum Reprod. 2008 Jan;23(1):105-11. DOI: 10.1093/humrep/dem257. Epub 2007 Nov 2. PMID: 17981820.
- Barbuscia A, Mills MC. Cognitive development in children up to age 11 years born after ART-a longitudinal cohort study. Hum Reprod. 2017 Jul 1;32(7):1482-1488. DOI: 10.1093/humrep/dex102. PMID: 28541549; PMCID: PMC5850752.
