Did you just complete an IVF cycle and you had a high number of immature eggs?
In this article, you’ll learn
- what an immature egg is,
- what causes them, and
- what you can do about them.
What is an immature egg?
An immature egg is an ovum, or egg cell, that has not yet developed to a stage where it can be fertilized.
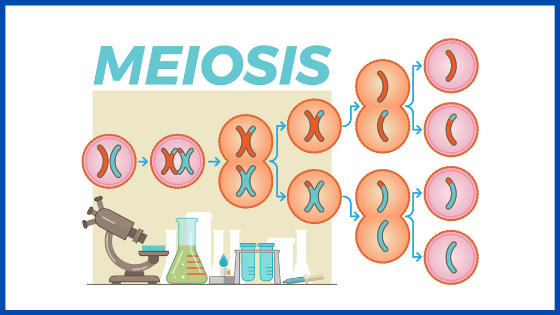
In order for an egg to “mature,” it needs to complete a process known as meiosis 1.
Meiosis 1 is when immature egg cells divide to become cells capable of combining themselves with another set of chromosomes (from the sperm).
If an egg does not complete meiosis 1, then that egg cannot be fertilized.
On average, we expect at least 15-20% of the total eggs collected in an IVF cycle to be immature.
Women with polycystic ovarian syndrome often have a higher percentage of immature eggs.
What causes immature eggs in ovaries?
In order for an egg to complete meiosis 1, it has to be exposed to a high level of Luteinizing Hormone (LH) while it is growing in the follicle.
The “LH surge” happens in a natural menstrual cycle (or the hCG trigger that we administer midway through an IVF cycle).
However, only the follicles that have reached a diameter of ~16-18mm will have the highest chances of yielding a mature egg,
The eggs that are in smaller follicles are unlikely to respond to the LH surge and will remain immature.
*Note: hCG stands for human chorionic gonadotropin. This is actually the pregnancy hormone, which very closely resembles Leutenizing hormone. This is why we can use it as a trigger instead of LH directly.
Can you get pregnant with immature eggs?
You cannot get pregnant with an immature egg because it does not have the proper number of chromosomes.
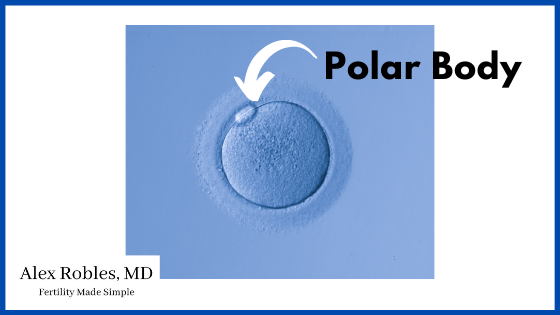
Immature eggs are diploid, meaning they contain 46 chromosomes. After the egg completes meiosis 1, it becomes a haploid with 23 chromosomes and extrudes the other 23 chromosomes into what we call a polar body.
(Cool fact- the presence of the polar body under the microscope is what tells us that an egg is mature).
The remaining 23 chromosomes are provided by the sperm.
What happens if an immature egg is fertilized?
Nothing will happen. Fertilization will not take place if a healthy sperm is injected into an immature egg as this combination will lead to an abnormal number of chromosomes.
What is the treatment for immature follicles?
There are a couple of things that can be done for immature follicles.
The first is in vitro maturation or IVM for short.
In Vitro Maturation
IVM refers to the maturation of immature eggs after their retrieval in the IVF laboratory. The hope is that the eggs will complete meiosis 1 outside of the body.
However, a high level of attrition is observed in eggs that have undergone IVM.
This means that they tend to have a lower chance of yielding a blastocyst embryo compared to eggs that were already mature at retrieval.
We think that is caused by incomplete cytoplasmic maturation (different from nuclear maturation which is what meiosis 1 does).
Unfortunately, we have no way of determining the cytoplasmic maturity of an egg.
More research is needed in this area to increase the efficiency of IVM for clinical use.
It is also important to note that not all IVF laboratories offer IVM for all patients. (IVM is an option often given to patients who are about to undergo cancer treatments and do not have an option of repeating another cycle).
Speak with your doctor to learn if you are a possible candidate for this
Optimizing The Next Cycle
The next option is only useful if you decide to do another IVF cycle. If you developed a high number of immature eggs, it may indicate that:
- You weren’t exposed to enough follicle-stimulating hormone
- Your follicles didn’t reach a big enough size to yield a mature egg, and/or
- Your eggs didn’t respond to the type of trigger shot used
In general, follicles that are at least 16-18mm in size have the best chance of producing a mature egg. However, some patients can have immature eggs despite having appropriately sized follicles.
In these cases, we may allow the ovarian follicles to get bigger (>19 mm for example) in a subsequent cycle to try and increase the likelihood of retrieving mature eggs.
In addition, we may try to increase the length of the IVF cycle to at least 8 days of stimulation (if your cycle happened to fall on the shorter side).
Lastly, we can try to use a “dual-trigger” approach, where we use both hCG and Leuprolide to induce a more robust surge in your body.
hCG provides a bolus of external hCG hormone (which is very similar to LH) while Leuprolide forces your pituitary gland to produce endogenous or internal LH hormone.
Unfortunately, there is no guarantee that any of this will work, and immature eggs may indicate something else going on contributing to your infertility.
Can ovaries release immature eggs?
Yes, your ovaries can release or ovulate immature eggs. The LH surge serves multiple purposes
- It helps to complete meiosis 1 of the larger follicles leading to extrusion of the first polar body
- It ensures that the smaller follicles die off to prevent multiple ovulation
- It causes ovulation
During an in vitro fertilization cycle, you will have more than one follicle growing at the same time. As a result, follicles that are greater than 10-12 mm in size can still ovulate despite not having reached nuclear maturity.
What are the symptoms of poor egg quality?
Unfortunately, there is no way to tell if you are producing immature eggs unless you complete an IVF cycle and undergo a retrieval.
You cannot detect an “immature egg” on an ultrasound or with a blood test.
There are no symptoms either.
What Are The Stages of Oocyte AKA Egg Development?
Oocyte Development (aka oogenesis) is the process that takes place in an ovary inside structures known as primordial follicles.
Through a series of steps, the primordial follicle develops into a
- primary follicle, then a
- secondary follicle, then a
- antral follicle, (these are the ones that are visible on transvaginal ultrasound)
- and then ultimately a Graafian or pre-ovulatory follicle.
Inside, the egg goes from a
- Germinal vesicle stage
- Metaphase 1 oocyte
- Metaphase 2 oocyte
The germinal vesicle is the “nucleus” of the egg which contains all the chromosomes /genetic material of the egg.
This germinal vesicle will then break down so that the egg can get ready to separate its chromosomes and extrude half of its chromosomes as a polar body. This is the metaphase stage of meiosis 1.
After the egg gets exposed to the LH surge, it completes metaphase and ultimately meiosis 1, to prepare for meiosis 2.
Meiosis 2 is completed at fertilization with a haploid sperm cell.
Final Words
Human eggs must undergo a series of nuclear steps to become a mature oocyte.
It is important to understand that almost all patients who undergo an egg retrieval will have immature eggs.
If you have an abnormally high percentage of immature eggs, be sure to speak with your doctor regarding any changes to your stimulation protocol.
Make An Appointment With Dr. Robles To Discuss Your Fertility Options Today!

Alex Robles, MD
Dr. Alex Robles is a Spanish-speaking Latino-American Reproductive Endocrinologist and Infertility specialist in New York City, and a board-certified OBGYN. He has a special interest in health, lifestyle, & nutrition. Make an appointment with Dr. Robles to discuss your fertility options today!
References:
- Plachot M, Belaisch-Allart J, Mayenga JM, Chouraqui A, Tesquier A, Serkine AM, Boujenah A, Abirached F. Qualité des ovocytes et embryons dans le syndrome des ovaires polykystiques [Oocyte and embryo quality in polycystic ovary syndrome]. Gynecol Obstet Fertil. 2003 Apr;31(4):350-4. French. doi: 10.1016/s1297-9589(03)00059-6. PMID: 12821065.
- IVM, OF. “In vitro maturation: a committee opinion.” Fertility and Sterility 115.2 (2021).

I was told that in a natural cycle and even with 5mg letrozole, that my follicles never become larger than 10mm. I do get positive LH strip and using basal body temperature charting my Temps indicate ovulation occurs around 95-98% of the time, yet I never get pregnant. My endometrial lining is trilaminar but only 5.3mm on average…and my period is very light, and spotting for 6-10 days each month …each cycle lasts about 25-28 days. I am 5’9, 140 lbs. I do not have multiple cysts as in a polycystic ovary, but I do get a lot of facial hair that I pluck. Not sure if that is pertinent, but I do not know why I never get mature follicles/sized 18mm or greater or what I could do about that?
Hi Tricia,
PCOS has many forms, and the ultrasound finding of a polycystic ovary is not needed for diagnosis. Patients with PCOS have chronically elevated levels of LH, therefore, LH strips aren’t as reliable in that patient population. If a follicle doesn’t exceed 10mm it is unlikely to be ovulating, let alone producing a mature egg. Spotting during the month can also indicate that ovulation is not occurring. I definitely recommend getting evaluated by a reproductive endocrinologist for a thorough assessment.